Bispectral Index Guided Target Controlled Midazolam Sedation
Abstract
Objectives: To assess the efficacy and safety of Bispectral Index (BIS) guided Target Controlled Infusion (TCI) of midazolam for anxiolysis or minimal sedation during extensive periodontal or implant surgery in a single operator/sedationist model.
Methods: Retrospective analysis of thirty adult ASA 1 or ASA 2 patients undergoing periodontal surgery or dental implant surgery under local anaesthesia were included.The calculated effect site concentration (Ce) of midazolam applied by TCI, BIS, heart rate (HR), and peripheral oxygen saturation (SpO2) were monitored continuously. Non-invasive blood pressure (NIBP) and mean arterial pressure (MAP) were measured every 10 minutes. All peri-operative parameters were recorded every10 minutes. All patients were interviewed 1 week after the procedure to explore their experience of sedation and the periodontal or implant surgery procedure.
Results: Extensive periodontal or implant surgery treatment in all 30 patients was completed in a mean time of 120 min (range 50-180 min). The calculated mean effect site concentration for midazolam was 50 ng/ml (range 24-80). The mean BIS was 85 (74-100) during induction and was maintained between 80 and 90 during the oral surgical procedure by adjusting TCI Ce. There were no clinically significant cardiopulmonary changes during midazolam infusion with regard to SpO2, NIBP, MAP and heart rate. Patients experienced profound anterograde amnesia and were very satisfied with the sedation and the surgical procedure.
Conclusions: BIS guided TCI sedation with midazolam facilitates predictable minimal sedation enabling long periodontal or implant surgery procedures by a single operator/sedationist within safe physiological limits.
Introduction
The main goal of sedation is to relieve anxiety, discomfort, and in facilitating dental care. Currently, several techniques for anxiolysis or minimal sedation are used in dentistry and consist of oral administration of benzodiazepines, inhalation of nitrous oxide, intranasal administration of midazolam, intravenous infusion of midazolam, or advanced techniques using intravenous propofol or multidrug therapy.1,2 Besides psychotherapeutic techniques and excellent local anaesthesia, prescribing oral benzodiazepines is the easiest technique for pharmacotherapeutic anxiety relief. However, it is rather difficult to prescribe the most suitable dose of a selected drug for the individual patient. In addition, it is difficult to provide a stable level of sedation for longer dental procedures with oral drugs.3 The intravenous route for administration of benzodiazepines surpasses this disadvantage of the oral route and facilitates better dosing by titrating the medication. Titration is a technique in which incremental small doses of drugs are injected until the patient is comfortable and without fear. The intravenous route also facilitates repeated injection of the drug during long treatment sessions. However, the manual nature of bolus injection gives variation of concentration of the drug, leading possibly to severe side effects compromising patient safety. Hence, intravenous bolus administration is not recommended for long dental surgery procedures. However, the intravenous technique can be improved by using continuous infusion of very low dosages of benzodiazepines.4 The aim of this study is to present a new technique of TCI midazolam minimal sedation with adjunctive BIS monitoring for long dental procedures by a single operator/sedationist.
Target Controlled Infusion (TCI) pumps
Drugs being used for sedation have to meet several conditions. The respective dosage needs to have a distinctive and predictable anxiolytic effect. The pharmacokinetic properties should facilitate titration of a wide range of sedation levels and the duration of action should be appropriate for the entire procedure. Sedation with manually titrated midazolam is used and is comfortable for procedures lasting up to 40-50 minutes. It is, however, suggested that alternative techniques, such as propofol used by anaesthesiologists or specially trained sedation practitioners, are used for extensive procedures.5
During manual titration of midazolam, the patient receives incremental numbers of low-dose bolus administration until the desired level of sedation is met. To compensate for pharmacokinetic changes during long treatment sessions, the patient will need incremental doses to provide a constant sedation level so manual titration may result in yo-yo type midazolam concentration and consequently sedation levels. Continuous administration of midazolam with a constant flow syringe pump might compensate for elimination and redistribution; resulting in a more stable plasma concentration. However, the redistribution from the central compartment is not a linear process. At the beginning, peripheral tissues do not contain any medication, so transfer of midazolam to these tissues will be much higher than after a period of time, when they are already filled with redistributed medication. Continuous syringe pumps will give a continuous infusion, but will not take into account the non- linearity of the transfer, resulting in high concentrations in the brain and thus deeper levels of sedation after longer periods of infusion. Because of a high risk of loss of consciousness, constant flow syringe pumps should never be employed in dental sedation practice to administer midazolam.
In 1996, the first TCI pump for propofol was introduced in anaesthetic practice.6 TCI means 'Target Controlled Infusion', in which a microprocessor automatically and variably controls the rate of infusion of a drug to attain a user defined target level in a (theoretical) effect site in the patient (usually blood or brain). The TCI pump will calculate:
- an initial bolus dose to fill the central (blood) compartment;
- a constant-rate infusion equal to the elimination rate from the blood compartment;
- a variable infusion that compensates for transfer from the central compartment to the peripheral tissues with an exponentially decreasing infusion rate.
Although, theoretically, the TCI technology based on pharmacokinetic models is available for almost any drug, the practical application of TCI is limited to drugs with a fast onset of the desired effect and short acting, like propofol or remifentanil.7,8 In general, these potent anaesthetic drugs are not considered suitable for the operator/sedationist in dentistry hence the TCI technique is not yet widely known in dentistry. In the current retrospective observational study we report our experience in the Netherlands with very low dose midazolam TCI guided by BIS, which we routinely use in our practice.
Monitoring the level of sedation
Sedation is a depression of a patient's awareness to the environment and reduction of responsiveness to external stimulation. According to the American Society of Anesthesiologists (ASA), the depth of sedation is a continuum of three sedation levels, followed by general anaesthesia (table 1).
Table 1 Continuum depth of sedation American Society of Anesthesiologists
- Minimal sedation is equivalent to anxiolysis, that is, a drug- induced relief of apprehension with minimal effect on sensorium.
- Moderate sedation is a depression of consciousness in which the patient can respond to external stimuli (verbal or tactile). Airway reflexes, spontaneous ventilation, and cardiovascular function are maintained.
- Deep sedation is a depression of consciousness in which the patient cannot be aroused but responds purposefully to repeated or painful stimuli. The patient may not be able to maintain airway reflexes or spontaneous ventilation, but cardiovascular function is preserved.
- General anaesthesia is a state of unconsciousness; the autonomic nervous system is unable to respond to surgical or procedural stimuli.
An older, but probably clinically more applicable measure of level of sedation is the Ramsay Scale (table 2).
Table 2 Ramsay Sedation Scale
- Patient is anxious and agitated or restless, or both
- Patient is co-operative, oriented, and tranquil
- Patient responds to commands only
- Patient exhibits brisk response to light glabellar tap or loud auditory stimulus
- Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus
- Patient exhibits no response
The level of sedation is determined by clinical observation. Preferably, the patient should stay at a pre-set sedation level during the entire treatment. Keeping patients in a conscious state is required to avoid airway and breathing problems or haemodynamic complications. In dentistry, intact protective airway reflexes are of even greater importance than in general medicine because cooling water is used and/or blood from wounds may flow into the oropharynx. Thus, maintaining swallowing and coughing reflexes are of vital importance during dental surgery. Dentists have to monitor the level of sedation on a continuous basis and the ability to communicate with the patient needs to be maintained. During long treatment sessions, clinicians are challenged providing incremental doses of medication or in case of TCI continuous effect site concentration to keep the patient as comfortable as possible but also keeping the patient awake. In the case of minimal sedation, a well-trained assistant should assist the dentist by monitoring the patient. We would clearly like to emphasise that during moderate and deep sedation the dentist cannot be responsible for providing sedation as well as the dental treatment, and that a separate well trained sedationist or anaesthetist is needed.
A BIS monitor can be used to monitor depression of the cerebral cortex. It measures electrical activity in the brain using an electroencephalogram (EEG). These EEG data are analysed and used to rank a patient’s level of brain activity on a Bispectral Index (BIS) of zero to 100, from coma to fully awake.9 In sedation practice with midazolam, the BIS monitor shows a very good correlation with level of sedation.10, 11
Pharmacology and pharmacokinetics of midazolam
Midazolam is water-soluble because the imidazole ring opens at a pH lower than 4. Injected into the circulation (pH about 7.4), this imidazole ring closes and midazolam becomes more fat-soluble, facilitating faster saturation into the nervous system and thereby resulting in a fast onset time (1.5-2 min). The redistribution halftime (Tα 1⁄2) after the first injection is 7-8 min. However, this time will increase when more midazolam is being injected for longer periods.4 In the liver, midazolam is hydrolysed into 1-hydroxy-midazolam by cytochrome P450 enzyme 3A3/3A4. Subsequently, the metabolites are glucuronidised and eliminated through the kidneys. The elimination halftime of midazolam (elimination from the body Tβ 1⁄2) is 1.8 to 2.5 hr and is influenced by drug interactions, older age, and liver or kidney dysfunction. As antidote, Flumazenil is available, a benzodiazepine missing any sedative effects which has a stronger affinity to benzodiazepine receptors on the cell surface then midazolam.
Material and Methods
Sample
We retrospectively analysed the initial 30 adult patients undergoing TCI midazolam sedation monitored by BIS during dental periodontal surgery or dental implant surgery lasting 50 min or longer. All patients were ASA 1 or ASA 2, older than 18 years and were informed in written form about conscious sedation and the operator/sedationist model. All patients were treated with the described TCI-BIS-guided midazolam minimal sedation technique; local anaesthetic articaine or lidocaine was used for infiltration in the upper jaw or mandibular block for pain prevention.
BIS Monitor
After cleaning the forehead, a sensor comprising 4 connectors was applied to the forehead and connected to the BIS monitor (Aspect BIS View monitor, Aspect Medical Systems Inc., U.S.A.). We used the BIS analysis to monitor changes of sedation levels, targeting BIS values between 80 and 90.12 We used an upper alarm set to 90 to prevent under-sedation, and a lower alarm set to 70 to prevent sliding slowly into moderate / deep sedation.
Perioperative Parameters
The effect site concentration (Ce), BIS, heart rate (HR) and peripheral oxygen saturation (SpO2) were monitored continuously, and non-invasive blood pressure (NIBP) was measured every 10 min. All measured variables and the calculated mean arterial pressure (MAP) were recorded every 10 min. When the saturation of a patient fell below 93%, the patient was stimulated to increase the frequency and depth of breathing. No patient received routinely supplemental oxygen because this can mask inadequate ventilation.13 However, oxygen was readily available to adequately treat the patient in case of oxygen desaturation.
Target controlled infusion pump and infusion scheme
A TCI-III pump (VERYARK Technology, China) was programmed with the pharmacokinetic model of midazolam.14 The use of the TCI pump was in accordance with a strict protocol. A 20 ml syringe was filled with 3 ml of 5 mg/ml midazolam which is commercially available in a 3 ml vial and diluted with 17 ml injectable 0.9% NaCl resulting in 20 ml of 0.75 mg/ml midazolam solution and the catheter was purged. The catheter was connected to a VenflonTM inserted into a vein of the antecubital fossa. The initial calculated target concentration in the brain was set to 30ng/ml and evaluated after 90 sec; after which the calculated effect site concentration was raised by 10 ng/ml every 60 sec, until the desired sedation level 2 of the Ramsay Sedation Scale (table 2) was reached. If patients intra-operatively showed deepening of sedation, tending towards moderate sedation, the pump was paused until the patient was again at the desired level of minimal sedation. Thereafter, the pump could be continued with a reprogrammed lower effect site concentration estimated by the pump itself. Usually 40 min before finishing dental treatment, the pump was stopped to allow for fast recovery.
Experience of treatment
After 1 week during consultation for suture removal, all patients were routinely interviewed regarding the experience of sedation and dental procedure. This was a non-structured open-ended interview about recollection of the treatment and satisfaction with the level of sedation.
Statistical analysis
Data analysis was performed with IBM SPSS statistics version 20. All continuous dependent variables were analysed by descriptive statistics with mean, and minimum/maximum.
Results
Patient sample and treatment time
A total of 30 patients (11 males and 19 females) were treated with BIS guided TCI midazolam minimal sedation (Ramsay 2) allowing extensive periodontal surgery or implant surgery with more patient comfort. Mean age was 53 years (28-73) and the mean treatment time was 120 min (50-180) (table 3).
Table 3 Descriptive of sample and perioperative parameters
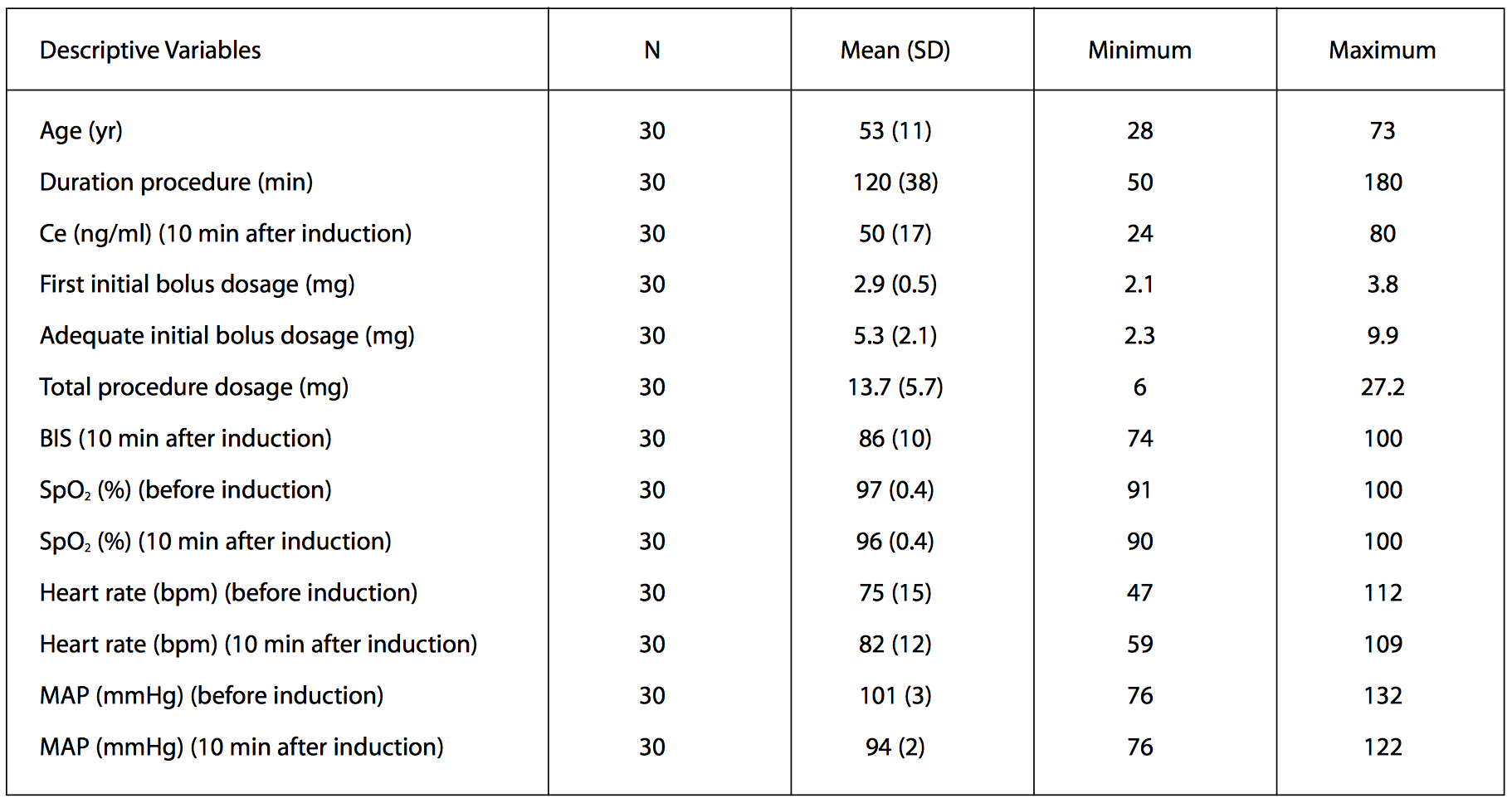
Target effect site concentration and bispectral index
Mean target effect site concentration of 50 ng/ml (24-80) was required for inducing adequate anxiolysis or minimal sedation (table 3 and figure 1). The BIS generally decreased to a mean of 85 (74-100) within the first 10 min. In most patients, the initial effect site concentration could be continued for the entire procedure and the BIS stayed between 70 and 90 for the rest of the treatment period (table 3 and figure 2).
Figure 1: Effect site concentration of midazolam (ng/ml) recorded every 10 min
Figure 2: Bispectral index (BIS) measured continuously and recorded every 10 min
Perioperative Parameters
The SpO2 data are shown in figure 3. This group of patients show an initial decrease of SpO2 to 96% during start of sedation, after which stable conditions were obtained (table 3). As shown in figure 3, the lowest value of SpO2 in all 30 patients was 90%.
Figure 3: Peripheral arterial oxygen saturation SpO2 (%) measured continuously and recorded every 10 min
Heart rate slightly increased at the start of sedation from 75 to 82 bpm and was from then on stable during the procedure (table 3 and figure 4). Mean arterial pressure decreased from 101 to 94 mmHg and a blood pressure increase was noted during periods of discomfort or pain (table 3 and figure 5).
Figure 4: Heart rate (bpm) measured continuously and recorded every 10 min
Figure 5: Mean arterial pressure (MAP,mmHg) measured every 10 min
Recovery
All patients were fit to leave the dental office after completion of the treatment and a minimum of 60 minutes after stopping midazolam injection. They were discharged into the care of a responsible adult escort.
Experience of treatment
A routine open-ended interview after one week, revealed that almost all patients experienced strong anterograde amnesia and did not have any specific memories regarding the procedure. Patients were very satisfied with the sedation as a comfortable way of treatment.
Complications
No significant cardiopulmonary complications were observed with regard to SpO2, NIBP, MAP and heart rate.
Noteworthy is one patient (age 73) who became deeply sedated with BIS of 58. After pausing the infusion pump and waking the patient, the pump was continued at the respective effect site concentration of 24 ng/ml. Subsequently, the sedation of this patient was stable and uneventful. No flumazenil was used in any patient.
It was noted that a sudden increase of BIS values was correlated with pain or increasing levels of noise, e.g. the use of an ultrasonic scaler. Where pain was experienced we improved the local anaesthesia, resulting in relaxation of the patient and dropping BIS values.
Discussion
We here report our first 30 patients treated using BIS-guided TCI minimal intravenous sedation by midazolam alone during long periodontal surgery and/or long implant surgery, extending from 50 min up to 3 hr. The main finding in this retrospective observational study is that all patients were effectively minimally sedated with adequate anterograde amnesia and no significant disturbances of cardio-pulmonary vital parameters. All patients were very satisfied with the sedation and the surgical procedure.
In the past, several authors have claimed that short dental treatments lasting up to 40 min can be treated with intermittent boluses of midazolam. However, during longer procedures, midazolam alone was believed to be inadequate and several alternative techniques like propofol continuous infusion or multidrug regimens are being used successfully in dentistry by specially trained personnel (anaesthesia nurses, sedation specialists, anaesthesiologists).
In a study by Craig et al.5, 20 patients received incremental titrated initial boluses of midazolam to an ideal conscious sedation endpoint, followed after 30 min by adjusted infusion rates of
200 mg/h propofol by a sedationist. All implant surgeries lasting between 55 and 160 min were carried out successfully. Total midazolam dosage for adequate initial sedation varied between 5 and 14 mg. In comparison with our observed cohort, our mean initial bolus was 2.9 mg (range 2.1-3.8 mg) and was titrated up to a mean 5.3 mg (range 2.3-9.9 mg) for adequate initial sedation. Continuing target-controlled infusion of midazolam reached a mean total dose of midazolam 13.7 mg (range 6.0-27.2 mg) for surgery lasting between 50 and 180 min. Craig et al.5, used a supplemental dosage of propofol between 25 mg and 375 mg. Throughout the surgery, arterial oxygen saturation was between 92% and 100% (without supplementary oxygen being administered), comparable to our cohort. All patients were fit for discharge within 20 min of termination of the propofol infusion.5
The group of Chrisp et al.15 utilised a dedicated registered nurse- anaesthetist for controlling TCI propofol/remifentanil and monitoring the patients. In their observational study, 150 patients were treated for oral surgery procedures. They found a high level of patient satisfaction and consistently good to excellent operating conditions. In their cohort, a higher BMI and male sex were associated with Oxygen Desaturation Events (ODEs), defined as a drop in peripheral oxygen saturation below 94%. However, oxygen was administered continuously via a nasal cannula running at two litres/min in all patients.15 Because oxygen inhalation might mask ventilation disorders, we did not give oxygen on a routine basis.
We strongly believe and advise that dentists should avoid using potent anaesthetics or multiple drugs for minimal sedation when only a trained dental assistant is available for monitoring. Therefore, in the current investigation, our aim was to optimise the operator/sedationist model with midazolam alone for longer procedures. Midazolam is a well-documented benzodiazepine with a wide margin of safety and it has the advantage of the availability of a reversal agent, Flumazenil. Lastly, midazolam seems to have better anterograde amnesia properties for pain then propofol during minimal sedation.12
As with any medical procedure, periodontal or implant surgery under sedation involves a certain amount of patient risk. A large part of this risk stems from the potential of sedation-related complications. However, patient selection, slow induction of sedation and careful monitoring of the sedation level can significantly reduce these risks. Cardiopulmonary events related to sedation and analgesia are the most frequent cause of dental sedation related morbidity and mortality. These complications range in severity from transient, minor oxygen desaturation, to life threatening events such as apnoea, shock/hypotension and myocardial infarction. Severe complications are extremely rare in dental minimal sedation and we therefore focus in our study on surrogate endpoints of morbidity: oxygen saturation, non-invasive blood pressure and heart rate. For measuring oxygen saturation we used a pulse oximeter with the lower alarm level set to 93%. Because affinity and dissociation of oxygen to haemoglobin is described by a sigmoid curve and not linear, oxygen saturation declines slowly from 100% to 90%. However, below 90% desaturation deteriorates much more rapidly. Setting a lower alarm to 93% gives the clinician time to correct the underlying cause of hypoventilation. We did not routinely administer supplemental oxygen. Besides preventing oxygen desaturation, supplemental oxygen also delays recognition of hypoventilation or apnoea.13 In our study early detection of hypoventilation and/or apnoea prevented, in all patients, oxygen saturation from falling below 90%. In future studies it would be advisable to also include capnograpy for early detection of a reduced respiratory rate.
Bispectral Index correlates well with several sedation scales.10 We used an upper alarm set to 90 to prevent under-sedation, and a lower alarm set to 70 in order to prevent sliding slowly into moderate /deep sedation. Especially during long procedures, downward and upward trends in BIS assisted our team in observing sedation levels even more closely and therefore a more consistent level of sedation could be maintained due to a more satisfactory titration of target effect-site concentration. In future research it would be interesting to test the clinical value of the upper and lower alarm value settings.
Compared to manual bolus titration of midazolam, the described TCI-BIS technique is quite complicated to learn. Also, utilising more equipment increases the chance for human error as well as functional failure of equipment. So, the practitioner should always have a backup plan.16 Hence, the described method is not a technique for the novice. An initial set of prerequisites would be an adequately trained team in sedation and training in advanced life support (ALS) by the dentist, and training in basic life support (BLS) by the dental assistant. Also, the dental assistant who is responsible for monitoring vital signs of the patient must only carry out small additional tasks.17,18 This training level is according to the Dutch guidelines and we are aware that the guidelines in the UK require immediate life support (ILS) for both the dentist and the dental assistant. Probably, a more advanced training of our dental assistants would improve our safety standards even more. In the Netherlands, there is currently debate about ILS training for the dentist, which is an easier training compared to the ALS requirement at the moment. It would be interesting to have more scientific proof rather than expert opinion regarding the appropriate training levels of the team.
Before commencing training in TCI with a mentor who is fully qualified, the clinician should be confident in providing stable minimal sedation for longer than one hour with manual repeated bolus midazolam.
The described TCI-BIS minimal sedation technique with midazolam has advantages and enables dentists treating anxious patients with extensive long invasive procedures in an equable comfortable state of mind. Possibly, the technique can be included in future UK guidance as a suitable alternative technique for single operator/sedationist.
Conclusion
This study shows proof of the principle that in this small series of 30 patients, BIS guided TCI sedation with midazolam facilitated predictable minimal sedation so enabling long periodontal or implant surgery procedures to be carried out by a single operator/sedationist within safe physiological limits.
References
1. Wilson K E, Dorman, M L, Moore, P A, Girdler, N M. Pain control and anxiety management for periodontal therapies. Periodontol 2000 2008; 46: 42-55.
2. Flick W G, Katsnelson A, Alstrom H. Illinois dental anesthesia and sedation survey for 2006. Anesth Prog 2007; 54: 52-58.
3. Dionne R A, Yagiela, J A, Coté C J, et al. Balancing efficacy and safety in the use of oral sedation in dental outpatients. J Am Dent Assoc 2006; 37: 502-513.
4. Fragen R J. Pharmacokinetics and pharmacodynamics of midazolam given via continuous intravenous infusion in intensive care units. Clin Ther 1997; 19: 405-419.
5. Craig D C, Boyle C A, Fleming G J P, Palmer, P. A sedation technique for implant and periodontal surgery. Journal of Clinical Periodontology 2000; 27: 955–959.
6. Mirakhur R K, Morgan M. Intravenous anaesthesia: a step forward. Anaesthesia 1998; 53: 1–3.
7. Gepts E. Pharmacokinetic concepts for TCI anaesthesia. Anaesthesia 1998; 53: 4–12.
8. Milne S E, Kenny G N C. Future applications for TCI systems. Anaesthesia 1998; 53: 56–60.
9. Sigl J C, Chamoun, N G. An introduction to bispectral analysis for the electroencephalogram. J Clin Monit 1994; 10: 392-404.
10. Cheung C W, Irwin M G, Chiu W K, Ying C L. A study to assess the value of bispectral analysis in intravenous sedation with midazolam during third molar surgery under local anaesthesia. Anaesthesia 2008; 63: 1302-1308.
11. Shah P, Manley G, Craig D. Bispectral index (BIS) monitoring of intravenous sedation for dental treatment. SAAD Dig 2014; 30: 7-11.
12. Matsuki Y, Ichinohe T, Kaneko Y. Amnesia for electric dental pulp stimulation and picture recall test under different levels of propofol or midazolam sedation. Acta Anaesthesiol Scand 2007; 51: 16-21.
13. Keidan I, Gravenstein D, Berkenstadt H, et al. Supplemental oxygen compromises the use of pulse oximetry for detection of apnea and hypoventilation during sedation in simulated pediatric patients. Pediatrics 2008; 122: 293-298.
14. Greenblatt D J, Locniskar A, Ochs H R, Lauven P M. Automated gas chromatography for studies of midazolam pharmacokinetics. Anesthesiology 1981; 55: 176-179.
15. Nagels A J, Bridgman J B, Bell S E, Chrisp D J. Propofol-remifentanil TCI sedation for oral surgery. N Z Dent J 2014; 110: 85-89.
16. Farbood A, Kazemi A P, Akbari K. Unintended purge during the start-up process of a syringe pump: report of a case presented with vascular collapse. J Clin Anesth 2010; 22: 625-626.
17. van den Berg T H, Preckel B. Intravenous light sedation with midazolam by dentists. Ned Tijdschr Tandheelkd 2014; 121: 617-625.
18. Preckel B, van den Berg T H. Safety of intravenous sedation with midazolam for dental treatment. Ned Tijdschr Tandheelkd 2015; 122: 247-249.